Herpes Simplex Infection
Explained In Simple Terms
If you’re new to the world of diseases, you would probably think herpes is just a sexually transmitted disease when it can actually refer to a family of viruses that manifest differently. For now, let’s focus on Herpes Simplex.
What is Herpes Simplex
Herpes simplex is a common viral infection caused by the herpes simplex virus (HSV). There are two main types:
HSV-1 is usually associated with oral herpes. It causes cold sores or fever blisters around the mouth. Take note that even if the symptoms are on the mouth, it can also cause genital herpes.
HSV-2 is primarily associated with genital herpes. It causes sores on the genitals or rectum but can spread up to the thighs. Though less likely, it can also cause oral herpes.
Once you get infected, the virus stays in your body for life. It can hide in nerve cells and reactivate periodically, leading to outbreaks of symptoms.
How is it Transmitted?
Herpes simplex is transmitted through direct skin-to-skin contact with someone who has the virus, especially during an outbreak when sores are present. However, it can also be transmitted when no visible sores are present. This is called asymptomatic shedding.
Oral herpes (HSV-1) is often spread through kissing, sharing eating utensils, or other close contact. Many people acquire HSV-1 during childhood.
Genital herpes (HSV-2, or sometimes HSV-1) is primarily transmitted through sexual contact, including vaginal, anal, or oral sex.
What Are The Symptoms?
Symptoms can vary greatly from person to person. Some people never experience symptoms, while others have frequent outbreaks.
First Outbreak (Primary Infection): This can be the most severe. Symptoms often include painful blisters or sores at the site of infection (mouth, genitals, rectum), which eventually crust over and heal. You might also experience flu-like symptoms such as fever, body aches, headache, and swollen lymph nodes.
Recurrent Outbreaks: Subsequent outbreaks are usually milder and shorter than the first. Before sores appear, you might feel tingling, itching, or burning in the area. This is called a prodrome. The sores typically heal within a week or two.
Where Do The Sores Appear?
Oral: Sores usually appear on the lips, around the mouth, or occasionally inside the mouth.
Genital: Sores appear on the penis, scrotum, vulva, vagina, cervix, buttocks, or inner thighs.
How To Manage It?
While there’s no cure, herpes simplex can be effectively managed.
Antiviral Medications: Medications like acyclovir, valacyclovir, and famciclovir can:
Shorten the duration and severity of outbreaks if taken at the first sign of symptoms.
Reduce the frequency of outbreaks if taken daily as suppressive therapy.
Reduce the risk of transmission to partners.
Pain Relief: Over-the-counter pain relievers (e.g., ibuprofen, acetaminophen) can help with discomfort.
Self-Care: Keep the affected area clean and dry, wear loose clothing, and avoid touching the sores to prevent spreading the virus.
Stress Management: Stress can be a trigger for outbreaks, so finding ways to manage stress can be helpful.
Could There Be Complications?
While generally not life-threatening, herpes simplex can lead to certain complications like:
Recurrent, painful outbreaks
Emotional distress, anxiety, or depression due to the stigma
Neonatal Herpes. If a pregnant person has active genital herpes during childbirth, the virus can be transmitted to the baby, which can be life-threatening for the newborn. C-sections are often recommended if there are active lesions during labor.
Other Infections because the sores can become infected with bacteria.
Ocular Herpes. In rare cases, HSV can infect the eyes, potentially leading to vision problems or blindness if not treated promptly.
Encephalitis/Meningitis. Although rare, herpes can cause inflammation of the brain (encephalitis) or the membranes surrounding the brain and spinal cord (meningitis), which are serious conditions.
Common Triggers That Reactivate The Virus?
Stress: Emotional or physical stress (like work pressure or anxiety) is the top trigger. It raises cortisol levels, weakening immunity temporarily.
Illness or Fatigue: Colds, flu, fevers, or exhaustion can spark an outbreak as your body fights other infections.
Sun Exposure: UV rays from sunlight (especially on the lips for oral herpes) can trigger cold sores. Lip balm with sunscreen helps prevent this.
Hormonal Changes: Menstruation, pregnancy, or starting/stopping birth control can shift hormones and prompt reactivation.
Physical Trauma or Friction: Skin irritation from tight clothes, waxing, or sexual friction (for genital herpes) can irritate nerves.
Weakened Immunity: Conditions like HIV, chemotherapy, or medications (e.g., steroids) make reactivation more likely.
Diet and Lifestyle: Foods high in arginine (like chocolate, nuts) or alcohol might contribute in some people, though evidence varies.
Outbreaks often start with a prodrome—tingling, itching, or burning 1-2 days before sores appear. Recognizing this early lets you start antivirals quickly to shorten it.
How to Prevent It?
Prevention focuses on avoiding contact with the virus, especially during outbreaks:
Avoid contact during outbreaks. Do not kiss or engage in sexual activity if you or your partner has visible sores or is experiencing prodromal symptoms.
Use condoms. While not 100% effective (as sores can appear in areas not covered by a condom), consistent and correct use of condoms can reduce the risk of genital herpes transmission.
Dental Dams. These can be used during oral sex to reduce transmission.
Disclosure. If you have herpes, it’s important to talk openly and honestly with your sexual partners about your status.
Antiviral suppressive therapy. For individuals with recurrent genital herpes, taking daily antiviral medication can significantly reduce the risk of transmitting the virus to partners.
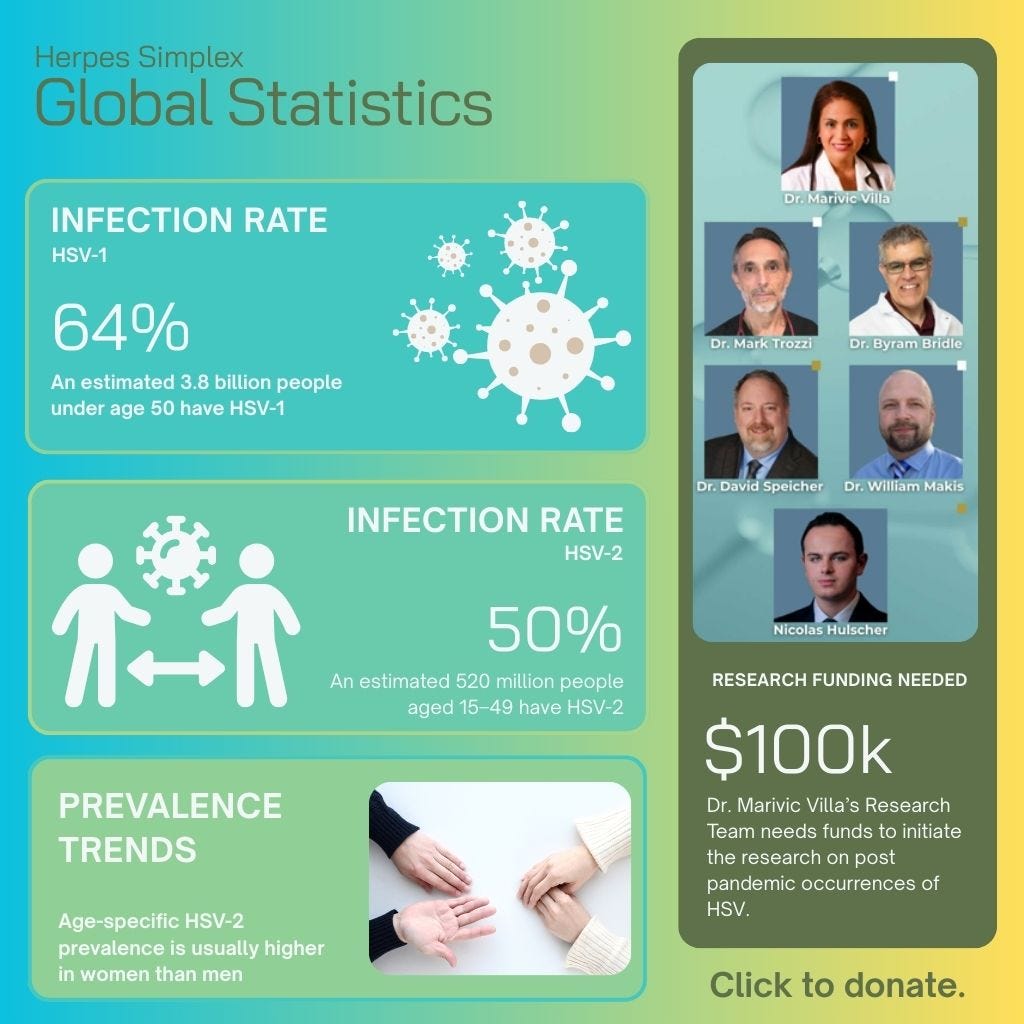
Herpes Simplex is just one kind of Herpes virus. More studies need to be done to stop the recurrences especially after the pandemic.
Dr. Marivic Villa’s research team is studying the current state of our immune system to help other doctors diagnose post pandemic illnesses faster. This is crucial for proper treatment protocols that can address diseases safer and quicker. If you’d like to support this research project, please donate and share this article.
Feel free to subscribe to World Council for Health Florida’s Substack for more articles like this.